Evolving Roles and Competencies in Healthcare Leadership
Changing Roles
Over the past 18-24 months the leadership ranks of healthcare organizations have witnessed proliferation of new roles or highly altered traditional ones, carrying a bewildering array of novel titles. In fact, the trend has advanced to the point that a few organizations have even jettisoned the CEO title. Examples of new or evolving senior roles gaining currency include:
- Chief Administrative Officer
- Chief Experience Officer/Patient Rights Officer
- Chief Quality Officer
- Chief Integration Officer
- Chief Clinical Transformation Officer
- Chief Data or Analytics Officer
This new landscape encompasses a blurring or reversal of conventional job paths as well. A recent story featured a hospital President/COO with a nursing background and extensive executive experience – yet never as a CNO.(1) Existing roles are undergoing evolutionary scrutiny. For example, one analyst noted that “new thinking is swirling around the CMIO role; the position is becoming increasingly matrixed, embedded in the IT department and doesn’t necessarily have direct reports.”(2)
Increasing Executive Turnover
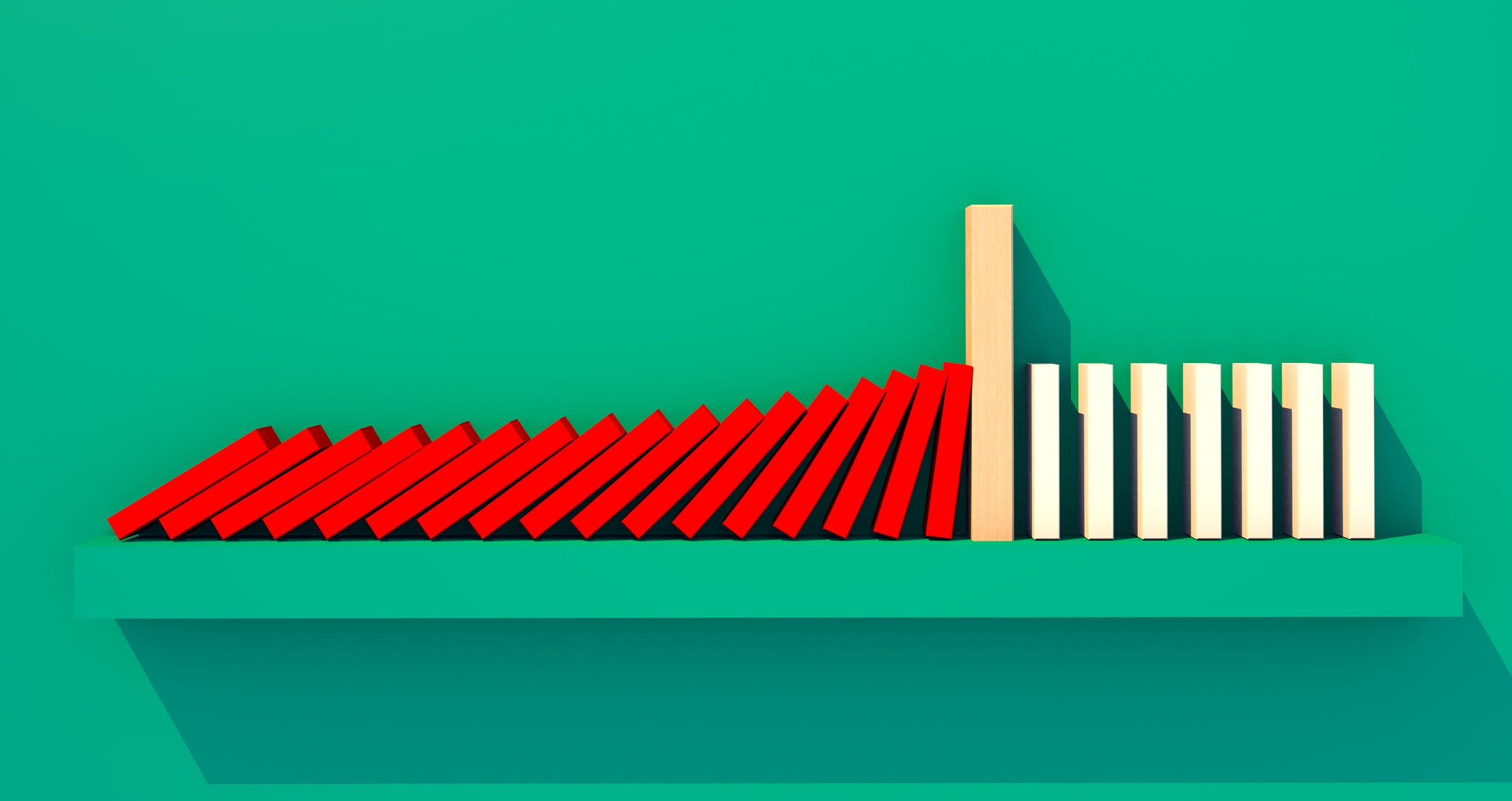
It is no coincidence that these role shifts and redefinitions are being accompanied by an uptick in leadership turnover. A new survey by the American College of Healthcare Executives (ACHE) found hospital CEO turnover at 18% in 2014. While it is lower than the record high of 20% in 2013, it still remains one of the highest recorded turnover rates in more than 30 years. In fact, the 18% rate has been recorded four times since 1981, and surpassed only once. In the report, ACHE’s president and CEO noted that “elevated turnover among hospital CEOs seems to be a feature of the current healthcare environment.”(3) While some of this movement is attributable to normal retirement decisions and hospital M&A activity, there are executives who make the decision to step down based on new roles or the need to navigate a rapidly changing industry.
This top level turnover carries significant ramifications that add to an organization’s leadership challenges. B. E. Smith research uncovered the following crucial effects of CEO departures:
What’s Driving Role Evolution?
Healthcare continues to pursue the value equation, undergoing a long-term transformation of its fundamental business model from one that relies on reimbursement for volume of procedures performed to one based directly on quality outcomes at a given cost level. This transformation is inducing major steps, from vertical and horizontal industry consolidation to deep costcutting to entrance of disruptive new market participants such as retail clinics. Healthcare organizations are becoming increasingly complex. Executive roles and responsibilities are hardly likely to remain static in such an environment.
The acceleration of role evolution is also a response to the industry entering a phase shift from investment and preparation to realization. It may be that 2015 marks the beginning of the “period of payoff.” Boards are looking for demonstration of return on investment in EHRs, in ACO/HIE participation in light of those structures’ uncertain economic models, and in a host of other major commitments of the past few years. Moreover, 2015 is the year federal incentives turn into penalties.
Emerging Competencies and Skill Sets
Whether the titles change, rapidly evolving roles carry with them a whole set of competency requirements - some classic, many new - for effective leadership. Traditional distinctions between leadership and functional skills or operations and strategy are breaking down in favor of new skill blends. In addition, competencies must be built on a foundation of four core leadership traits: Intellect, Interpersonal Ability, Integrity and Intensity.
It is imperative that current and prospective leaders not just enumerate skills needed for given roles, but also understand the complex interplay of demands.

The following competencies are requirements common to many of the new roles:
Continuous planning. Strategy is an “always on” activity today. Leaders may establish a long-term framework but they must be constantly assessing and adapting it in a world where high uncertainty and low control reigns. As a McKinsey report notes, “this means monitoring trends, engaging in regular scenario-planning exercises, wargaming the effects of potential disruptions…”(4)
Driving and managing innovation. Change is the highest level strategic imperative. This mandate is difficult because healthcare has historically not been an aggressively innovative industry and most of its executives have little training in the techniques of fostering innovation. Today’s effective leader must pull several change management levers simultaneously:
- Favor the disruptive over the incremental.
- Recognize that innovation goes beyond the senior team. Every supervisor and every level of management today must participate in innovation and change management. The IT department can no longer adopt the traditional implementer/technical expert stance; finance has to embrace clinical understanding to drive true cost changes. Top management should seek ways to permeate the organizational culture with a sense that it is “safe to disrupt.”
- Make tough tradeoffs. Today’s constrained environment requires projects and initiatives to undergo strict scrutiny, ensuring the focus remains on delivering high level patient care and achieving the best results for the organization.
Rapid decision making. Bringing a real sense of urgency and nimbleness to the decision process is vital. Organizations no longer possess the luxury of time they once did. Critical market opportunities must be seized and underperforming units or service lines usually need to be closed quickly. Interestingly, this fast-decision environment can be challenging for some leaders of the “baby boomer” generation, whose business career and experience tended to reward deeper analysis and more measured strategies.
Ability to deal with ambiguity. Change can be “messy” with unproven choices on the table (HIE, new alliances) and a context that can lack clarity, as evidenced in a recent B. E. Smith survey that found 47% of executives feeling “highly uncertain” or “uncertain” about 2015.(5) We again find generational differences here with some of the younger staff exhibiting greater comfort with non-linear, less predictable pathways and choices.
Soft skills. These three “soft skills” are becoming indispensable for emerging roles:(6)
- Agility and Adaptability
- Communication and collaboration skills to manage relationships with a wide range of internal and external constituencies, fulfill contemporary expectations of transparency and articulate persistently the vision for change.
- Ability to inspire. Leading today is as much through influence as through authority.
Courage and honesty. Given the trend toward a centralized, integrated corporate model for healthcare delivery to gain control of outcomes and produce value, leaders need an honest assessment of their organizations’ long-term prospects and comparative capabilities. For leaders today, this includes considering merger, alliances or other transformative steps.
Building physician leadership. B. E. Smith has experienced a significant increase in requests to recruit physicians to the leadership suite as organizations seek clinical/administrative alignment. These physician leaders must bring forward the same competencies and traits as other executives, particularly the ability to drive change. As one analyst observes, “Hospitals and health systems are looking for physicians with innovative ideas … to view the care delivery process not only through the eyes of the provider, but also of the patient…”(7) Physician executives must also possess managerial and financial skill sets required to successfully lead healthcare organizations. For this reason, many physicians have obtained MBAs or MHAs to complement their medical degrees.
Enriching the Understanding of Competencies
The story of emerging roles goes beyond the growing list of skills and traits. A deeper understanding takes into account several additional considerations regarding success. First, remember that each leadership competency encompasses many specific attributes – or “micro-skills” - that require attention and training, especially for developing new leaders. Also, the list of desirable attributes is not static, so organizations need to be envisioning not just competencies of today, but of tomorrow as well.
Second, leaders must possess the self-awareness to recognize they will not exhibit “five star” capability on all skills. The best leaders determine what they are good at and then surround themselves with people who bring exceptional skills in other strategic and tactical areas. Outside consultants can often bring objective help to this assessment process.
Third, leaders must perform a balancing act. Think of the competency sets as a portfolio in which skills are emphasized or deemphasized as different situations dictate. For example, while pressing forward on innovative strategies, urgent financial conditions may elevate attention to cost and revenue as a priority. A related modulation involves setting the appropriate pace of change for the organization within an overall context of speed of execution. Disruption is a relative term. Some hospitals exist in highly competitive markets and must exhibit disciplined hyper-agility. Others are in more protected or smaller markets, where leaders must guard against complacency and the danger of not moving fast enough to adapt.
Strategies to Manage Leadership Evolution
B. E. Smith’s ongoing leadership development advisory provides a window onto fresh approaches and best practices to navigate emerging and new roles:
- Consider recruitment from less traditional backgrounds and outside the industry. Some organizations continue to seek traditional competencies and executive experience, overlooking less conventional but more forward-thinking candidates. The importance of widening the search scope is underscored by the fact that the supply of people with the competencies for future successful leadership trails the industry’s projected demand. B. E. Smith has experienced successful examples of the nontraditional approach, such as a CEO whose background consisted of process engineering in the computer industry. This individual proved to be a creative, problem-solving healthcare executive who could induce change.
- Develop leaders using new/alternative career paths and interdisciplinary education. With care moving outside the historical institutional boundaries, leaders need to be externally as well as internally focused. Create meaningful opportunities for exposure to inpatient, outpatient and post-acute settings whenever possible. Seek ways for potential leaders to gain understanding of departments, functions and roles beyond their core domains.
- Employ coaching and interim management. Executive mentoring and coaching can be especially helpful to onboard both new and experienced leaders, who are faced with navigating a new culture and challenges. Options range from informal to formal programs and often involve a mix of inside and outside mentors. B. E. Smith finds that such assistance for executive leaders is often overlooked yet crucial. Organizations which utilize coaching or onboarding are more successful in retaining executives beyond the first 18 months of an appointment. When key leadership vacancies occur, interim management can go beyond serving as a caretaker and actually create or maintain strategic speed and momentum. During one of B. E. Smith’s interim engagements, for example, a hospital leader was able to execute a system-wide plan that reduced length of stay 11% in four months, saving over $1.5 million.
- Create leadership development metrics. Assessment tools exist to help measure key competencies. Examine if these tools are customizable, as off-the-shelf models tend to have limited value. Unfortunately, there are few reliable benchmarks to evaluate an organization’s progress on leadership role change and maturity of competency development. Working with industry peers and consultants often offers the best guide to real-world comparisons.
Conclusion
Given the scope and intensity of change confronting the industry, healthcare executive roles will continue to evolve at a fairly brisk pace. Managing this leadership change presents complex issues. Organizations which take a proactive and creative approach to this changing dynamic will build a winning leadership team ready to adapt not only to today’s challenges, but those yet to come.
Resources
- Alexandra W. Pecci, “Thoughts from a New Nurse COO,” HealthLeaders Media, January 13, 2015.
2. Rebekah Apple, “Evolution of the C-Suite,” Physician Executive Journal, May/June 2014.
3. “Hospital CEO Turnover Rate Remains Elevated,” ACHE, March 5, 2015. http://www.ache.org/pubs/Releases/2015/hospital-ceo-turnover-rate15.cfm
4. Dobbs et. al., “Management Intuition for the Next 50 Years,” McKinsey Quarterly, Sept. 2014
5. B. E. Smith Executive Survey, September 2014.
6. For a fuller discussion of these skills, see Madden, “Essential Soft Skills for Healthcare Leaders in the Era of Reform,” B. E. Smith white paper, 2014.
7. Rebekah Apple, “Evolution of the C-Suite,” Physician Executive Journal, May/June 2014.