10 Tips for a Successful CDI Program
- Providers should be involved in a CDI program initiative from conception and continue throughout its existence. If one considers the key operational figures in a CDI program, there are three – the patient, represented by a functional medical record, the provider, whose documentation is the primary link to the care provided, and the CDI professional, who reviews the medical record for precise and comprehensive documentation – it makes sense that without these three operational figures on board from the onset, it doesn’t matter how a CDI program is set up, the path for success is strewn with obstacles. Involving significant providers from the onset is crucial for program success.
- There are certain skills that the CDI professional must possess in order to succeed, and the first of these is clinical expertise. It’s crucial to understand disease pathways, anatomy and physiology and be able to critically think through scenarios in order to determine documentation integrity. Equally important is effective communication with providers. The CDI professional must be able to communicate the clinical skills they’ve acquired.
- Once a CDI professional’s clinical skills are at an expert level, their coding expertise must follow suit. Using the clinical evidence extracted from the medical record, the CDI professional’s knowledge of the Official Guidelines for Coding and Reporting and other official sources of rules and guidelines to ensure documentation integrity is paramount to CDI program success.
- Those outside the CDI (and the HIM) professional’s realm are always interested to know that there is an industry standard for asking a question of a provider. Questions posed to a provider, also called queries, can have an impact on documentation, coding and billing and possibly result in an erroneous depiction of the patient’s health status. As such querying the provider is a sensitive process that requires compliance with industry standards. By strictly following the ACDIS/AHIMA Practice Brief, Guidelines for Achieving a Compliant Query Practice (2019 Update), compliant querying will support CDI program success.
- A successful CDI program can maintain a high level of success with a quality initiative program. By regular reviews performed by unbiased CDI experts whose only goal is documentation integrity, the skill level of the CDI professional will remain strong despite ever-changing coding and billing guidelines, and ever-evolving medical best practices.
- A CDI professional is the gatekeeper of the medical record and holds to the role of assisting with comprehensive medical record documentation that precisely depicts the patient’s health status at the time of the encounter. Upholding the gatekeeper role, the CDI professional has an additional responsibility in helping to de-silo departments and bringing HIM, quality, compliance, case management, and denial departments together in their quest in support of the patient.
- Developing robust, complete policies and processes are integral to a successful CDI program. Written policies and processes are the strongest communication tool an organization can possess. A successful CDI program will reap effective communication benefits from the onset with a comprehensive orientation manual along with subsequent policies and processes.
- Risk adjustment has been a cornerstone of measuring outcomes for decades. The MS-DRG system, like the DRG system before, along with the APR-DRG system, operates on a limited risk methodology as they classify the patient according to CCs (Complications or Co-morbidities)/MCCs (Major Complications or Co-morbidities) and SOI (Severity Of Illness)/ROM (Risk Of Mortality), respectively. As risk adjustment methodology evolves, HCCs (Hierarchical Condition Categories) remain the most widely used methodology. This is an unlimited system which is considered to be the most reasonable and open methodology in the industry thus far.
- Clinical validation has always been an integral part of a CDI professions role, even though it didn’t have a “name” as such. Clinical validation can be defined as a clinical review of the medical record to verify documented conditions by applying widely accepted medical diagnostic standards. By applying their clinical expertise, a CDI professional will validate every diagnosis before moving to identification of the necessity of a clarification. By taking a strong approach to proactive clinical validation, denials will decrease. A successful CDI program will recognize and strengthen the CDI professional’s innate clinical validation skills.
- Last, and by no means least, and truth be told, first, is the patient. By paying homage to the patient and placing an accurate depiction of the patient first and foremost, the CDI program will be successful due to the fact that everything discussed thus far comes together in a comprehensive and precise medical record that is a true depiction of the patient’s health status.
Are you ready to initiate or expand a successful CDI program? AMN Healthcare has the experts to set your CDI program up for success!

Additional Revenue Cycle Resources:
- Cancer Registry: Learn about Cancer Registry careers and opportunities.
- Case Management Utilization Review: Join a team pairing decades of Revenue Cycle knowledge with the support of one of healthcare’s most trusted brands.
- Refer-a-Friend: Make up to $2,000 per referral.
Latest News
Case Study: Establishing a Strong Financial Foundation through a Commitment to Quality
Our recent cases study showcases how a healthcare organization in the South tackled issues with its quality scores and revenue by implementing a Clinical Documentation Integrity (CDI) program in
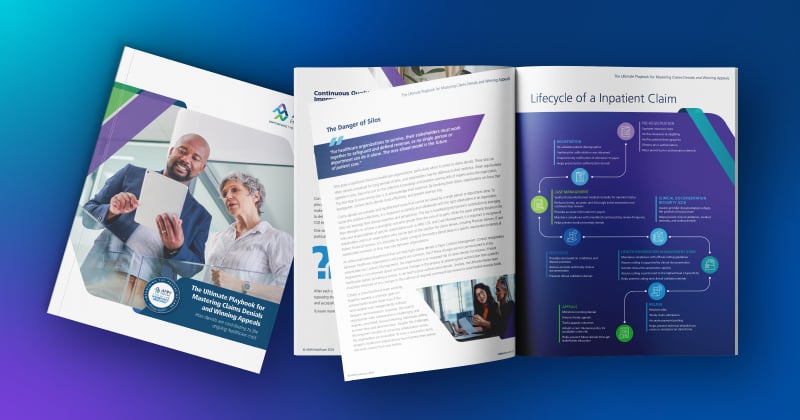
The Ultimate Playbook for Mastering Claims Denials and Winning Appeals
This comprehensive guide examines the complexities of appeals and denials and offers critical strategies for navigating toward a more financially stable future for healthcare organizations
Continuous Quality Improvement: Using the PDSA Cycle to Solve Claims Denials
One effective Continuous Quality Improvement (CQI) model is the PDSA (Plan-Do-Study-Act).
Webinar: Protecting Your Healthcare Data: Uncovering Vendor Cyber Security Threats
In this recorded webinar, you will discover how to safeguard your data, the top qualities to look for when selecting a secure vendor, and cyber security best practices to protect your valuable
Case Study: Advent Health Reduces Avoidable Days to Improve Patient Satisfaction & Drive Savings
Download the full case study to discover how AdventHealth partnered with AMN Healthcare Revenue Cycle Solutions (RCS).
3 Strategies for Cultivating a Culture of Connection, Development, and Loyalty in the Modern Workplace
Explore job satisfaction: Learn 3 strategies for fostering connection, development, and loyalty in our white paper.
Outpatient Clinical Documentation Integrity Solution
The current trajectory of U.S. healthcare points to the growing number of outpatient visits and procedures. As a result, alignment of quality measures, data accuracy, and revenue integrity are
The Five Pillars of Trauma Revenue
AMN Healthcare's Trauma Billing Program provides a method for recovering the cost associated with the Trauma Service and a pathway to a stronger financial future.