CDI & Coding Considerations for Myocardial Injury
Studies have shown that myocardial injury, defined by an elevated cardiac troponin (cTn) value, is frequently encountered clinically and is associated with an adverse prognosis. Although the myocardial injury is a prerequisite for the diagnosis of MI it is also an entity in and of itself. To establish a diagnosis of MI, criteria in addition to abnormal biomarkers are required. Non-ischaemic myocardial injury may arise secondary to cardiac conditions such as myocarditis or may be associated with non-cardiac conditions such as renal failure.
Therefore, for patients with increased cTn values, clinicians must distinguish whether patients have suffered a non-ischaemic myocardial injury or one of the MI subtypes. If there is no evidence to support the presence of myocardial ischemia, a diagnosis of myocardial injury should be made. This diagnosis can be changed if the subsequent evaluation indicates criteria for MI. The current Fourth Universal Definition of Myocardial Infarction Consensus Document reflects these considerations through adhering to the clinical approach of the definition of MI. (Fourth Universal Definition of Myocardial Infarction, 2018)
Even though a clinical diagnosis for an elevated cardiac troponin exists, this presents a significant CDI and coding challenge in ICD-10-CM. To begin, following the FY 2019 classification in search of myocardial injury we find:
Injury
Ø Myocardium – see Injury, heart
As we look up ‘Injury, heart’, it is noted they are all S26.- codes. These are traumatic injury codes and include codes for contusions and lacerations, none of which describe a myocardial injury as defined in the 4th UDMI.
So, the question becomes, what is the appropriate code to be assigned? The most important point to remember is that a code is not to be assigned if it doesn’t fit the scenario. This is stated in Coding Clinic 3Q 2017, pp 24-25. Even though the Coding Clinic is answering a question about emaciation and malnutrition, a significant point was designated in the answer, “…a basic rule of coding is that further research is done if the title of the code suggested by the Index does not identify the condition correctly.” Obviously, no one would assign a traumatic heart injury code (or any code for that matter) without considering the clinical scenario. During code assignment, there is going to be natural validation of the code and if the clinical evidence shows no traumatic injury, an S26 code would not be assigned.

Knowing that a traumatic heart injury code is not appropriate, we would next look at the definition of myocardial injury and consider a code for elevated cardiac troponin. Unfortunately, there is no specific code for an elevated cardiac troponin leaving us with the assignment of R74.8 Abnormal levels of other serum enzymes. This makes coding sense because troponin (a protein) is a type of enzyme. In fact, there is a ‘tip’ under code R74.8 that states, “Assign for documented abnormal or elevated troponin level when a definitive diagnosis has not been established.” However, even though we do have a definitive clinical diagnosis, we don’t have a codable diagnosis.
Following the guidance found in Coding Clinic 3Q 2017, equating myocardial injury, a definitive cardiac event to an abnormal lab value is not an appropriate code choice but until further advice in a Coding Clinic and/or code guidance is provided, this is what we have at this time.
While a traumatic heart injury code or an abnormal finding of blood chemistry code assigned for a myocardial injury is either inappropriate or not clinically relevant, neither should there be a myocardial infarction (MI) code assigned to a documented myocardial injury.
Based on the excerpt from the 4th UDMI that begins this blog, myocardial injury and myocardial infarction are two separate clinical entities and not a substitute for each other. Along with that same thought, caution needs to be emphasized regarding a Coding Clinic from 1992, 1Q, pp 9-10, Myocardial Injury without Myocardial Infarction, which leads us to assign a code for other acute and subacute forms of ischemic heart disease (I24.8 in ICD-10-CM).
Myocardial injury is not ischemic. This is clear in the 4th UDMI and therefore, the code title suggested by the index does not identify the condition correctly. The clinical information published in 1Q 1992 is outdated and not clinically relevant with recent best practice medicine. In addition, the 1Q 1992 Coding Clinic also provides clinical information and has repeatedly stated in various coding clinics, clinical information published in the coding clinics is not to be used as clinical criteria for code assignment. Based on the information in 1Q 1992 and 3Q 2017 Coding Clinics, caution is to be practiced if considering assigning a cardiac ischemia code to the documentation of a myocardial injury.
There are a lot of concerns regarding code assignment of non-traumatic myocardial injury at this time. Therefore, until further guidance is published, it is recommended that each facility have a roundtable discussion and invite cardiologists, hospitalists, medical leadership, CDI, HIM, and quality to discuss and establish a policy and procedure surrounding code assignment of non-traumatic myocardial injury.
Wishing you success in CDI!
Additional Revenue Cycle Resources:
- Cancer Registry: Learn about Cancer Registry careers and opportunities.
- Case Management Utilization Review: Join a team pairing decades of Revenue Cycle knowledge with the support of one of healthcare’s most trusted brands.
- Refer-a-Friend: Make up to $2,000 per referral.
Latest News
Case Study: Establishing a Strong Financial Foundation through a Commitment to Quality
Our recent cases study showcases how a healthcare organization in the South tackled issues with its quality scores and revenue by implementing a Clinical Documentation Integrity (CDI) program in
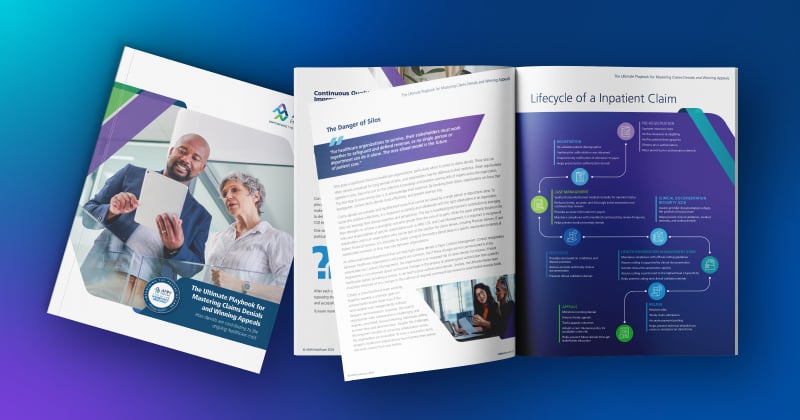
The Ultimate Playbook for Mastering Claims Denials and Winning Appeals
This comprehensive guide examines the complexities of appeals and denials and offers critical strategies for navigating toward a more financially stable future for healthcare organizations
Continuous Quality Improvement: Using the PDSA Cycle to Solve Claims Denials
One effective Continuous Quality Improvement (CQI) model is the PDSA (Plan-Do-Study-Act).
Webinar: Protecting Your Healthcare Data: Uncovering Vendor Cyber Security Threats
In this recorded webinar, you will discover how to safeguard your data, the top qualities to look for when selecting a secure vendor, and cyber security best practices to protect your valuable
Case Study: Advent Health Reduces Avoidable Days to Improve Patient Satisfaction & Drive Savings
Download the full case study to discover how AdventHealth partnered with AMN Healthcare Revenue Cycle Solutions (RCS).
3 Strategies for Cultivating a Culture of Connection, Development, and Loyalty in the Modern Workplace
Explore job satisfaction: Learn 3 strategies for fostering connection, development, and loyalty in our white paper.
Outpatient Clinical Documentation Integrity Solution
The current trajectory of U.S. healthcare points to the growing number of outpatient visits and procedures. As a result, alignment of quality measures, data accuracy, and revenue integrity are
The Five Pillars of Trauma Revenue
AMN Healthcare's Trauma Billing Program provides a method for recovering the cost associated with the Trauma Service and a pathway to a stronger financial future.