Detailing Dementia: FY2023 Code Expansion
This coming October 1st coding professionals must become familiar with the expansion details of reporting codes for dementia. This expansion was precipitated by a CMS initiative to gather clinical data on the care of dementia patients. The goal of data collection is to identify the stages of dementia when associated behavioral and psychological symptoms start to develop.
Other goals include reducing the use of antipsychotic medications favoring nonpharmacologic approaches and enhancing patient-centered dementia care practices (Source: CMS Contributors, 2022). The code categories impacted by this expansion are F01 Vascular Dementia, F02 Dementia in other diseases classified elsewhere, and F03 Unspecified dementia. Treating dementia revolves around treating the associated condition. The associated condition is what links to patient outcomes, impacting the quality of life, cost of care, institutionalization, and accelerated mortality.
Understanding the FY2023 Dementia Code Expansion
The first characteristic to become familiar with is the severity of dementia identified as mild, moderate, and severe. The following definitions are quoted directly from the ICD-10 Coordination and Maintenance Committee Meeting minutes of September 14-15, 2021. (Source: Bullock, 2021) Of note, these definitions are applied routinely by clinicians, professional societies, and advocacy groups such as the American Academy of Neurology, the American Geriatrics Society, the Gerontological Society of America, the National Society on Aging, and the Alzheimer’s Association.
- “Mild dementia: Clearly evident functional impact on daily life, affecting mainly instrumental activities. No longer fully independent/requires occasional assistance with daily living activities.”
- “Moderate dementia: Extensive functional impact on daily life with impairment in basic activities. No longer independent and requires frequent assistance with daily living activities”
- “Severe dementia: Clinical interview may not be possible. Complete dependency due to severe functional impact on daily life with impairment in basic activities, including basic self-care.”
The final characteristics to become familiar with are the associated behavioral and psychological conditions such as: agitation, psychotic disturbance, mood disturbance, and anxiety. In October 2011, the codes for dementia received an update signifying the presence of behavioral disturbances such as sleep disturbances, social disinhibition, sexual disinhibition.
Now, there is a need for additional detail regarding the behavioral and psychological symptoms of dementia (BPSD). It is important to know that patients can experience one or more BPSD with treatment strategies differing between disorders. Most patients with dementia will be afflicted with some form of BPSD. Collecting data on the associated conditions allows for the most appropriate interventions and development of new non-pharmacological and pharmacological treatments to improve adverse outcomes. There are three main types of BPSD discussed below.
The three types of associated conditions are: Agitation, psychosis, and mood.
Agitation is the most disruptive behavioral disturbance prompting Emergency Room visits and is a high risk for institutionalization. The International Psychogeriatric Association has identified agitation in dementia patients as distinctly different from how agitation presents in other populations.
The codes contain the inclusion terms:
- Aberrant motor behaviors such as restlessness, rocking, pacing, and exit seeking.
- Verbal or physical behaviors such as profanity, shouting, threatening, anger, aggression, and combativeness, violence.
Psychotic disorders associated with dementia are identified in the code inclusion terms as: hallucinations, paranoia, suspiciousness, and delusional state. Studies have shown a correlation between psychotic disorders and acceleration of cognitive decline and increased mortality.
Mood disorders associated with dementia are identified in the code inclusion terms as: depression, apathy (lacking emotion), anhedonia (decreased ability to feel pleasure). Studies have shown a correlation between mood disorders and lower quality of life scores.
Anxiety is a common BPSD and is more common in vascular and frontotemporal dementia than Alzheimer’s or Parkinson’s. Anxiety tends to gradually decrease at the severe stages of dementia.
(Source: Kwak et al., 2017)
Since a mild cognitive disorder or impairment can precede the diagnosis of dementia a new subcategory F06.7- for mild cognitive disorder has been added. Mild cognitive disorder may precede a diagnosis of dementia.
Patients with mild cognitive impairment (MCI) experience frequent memory deficits not expected for a particular age. This condition may progress to dementia, or it may be due to another medical condition or a medication issue.
These codes are:
- 70 Mild neurocognitive disorder due to known physiological condition without behavioral disturbance.
- 71 Mild neurocognitive disorder due to known physiological condition with behavioral disturbance.
The coder is advised with the instructional note to first code the underlying physiological condition such as HIV disease or Lupus.
Coding professionals have a great responsibility to capture the most specific codes. The data that will be researched regarding both dementia stage and the associated conditions will be invaluable in developing management strategies. Dementia is a progressive illness requiring longitudinal clinical data to move research and clinical studies forward.
Resources
Centers for Medicare & Medicaid Services. Contributors. (2022. July 29). National Partnership to Improve Dementia Care in Nursing Homes Retrieved, August 2, 2022. from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/National-Partnership-to-Improve-Dementia-Care-in-Nursing-Homes
Bullock, C. (2021, September 14). ICD - ICD-10-CM - coordination and Maintenance Committee. Centers for Disease Control and Prevention. Retrieved August 16, 2022, from https://www.cdc.gov/nchs/icd/icd10cm_maintenance.htm
Kwak, Y. T., Yang, Y. S., & Koo, M.-S. (2017, June). Anxiety in dementia. Dementia and neurocognitive disorders. Retrieved August 11, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6427954/

Additional Revenue Cycle Resources:
- Cancer Registry: Learn about Cancer Registry careers and opportunities.
- Case Management Utilization Review: Join a team pairing decades of Revenue Cycle knowledge with the support of one of healthcare’s most trusted brands.
- Refer-a-Friend: Make up to $2,000 per referral.
Latest News
Scheduling for Maximum Efficiency: A Comparison of 4, 6, and 8-Week Schedule Periods
Optimizing workforce management is crucial for delivering high-quality patient care while
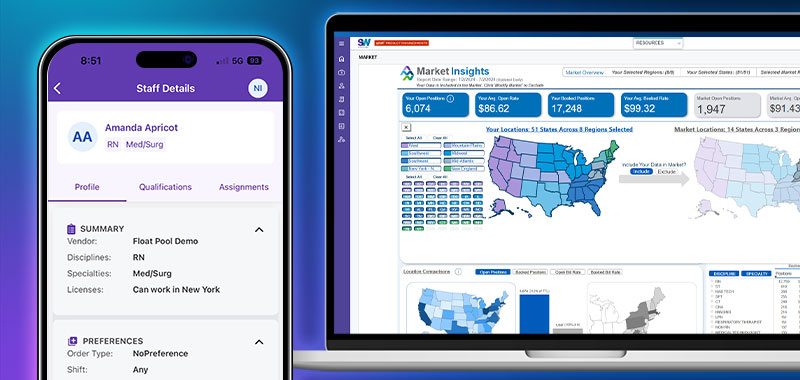
Enhanced Workforce Planning with Real-Time Insights
Workforce planning is a balancing act—juggling operational demands, financial targets, and the need for actionable insights.
Smart Square Named 2025 Best in KLAS for Nurse and Staff Scheduling
AMN Healthcare, the leader and innovator in total talent solutions for healthcare organizations, has been recognized with the 2025 Best in KLAS Scheduling: Nurse & Staff award for its industry
Understanding Turnover: A Study of Staffing and the Correlation to Turnover
By focusing on key staffing metrics like cancellations, overtime, and core staff floating, you can uncover actionable insights to transform your workforce strategy and retain top talent.
Revolutionize Your Locums Staffing with ShiftWise Flex
ShiftWise Flex is a cloud-based Vendor Management System (VMS) that offers comprehensive capabilities to manage healthcare professionals, including physicians, nurses, and allied health workers,
Optimize Staffing with Smart Square's Data-Driven Insights
Unlock the power of data with Smart Square's advanced reporting abilities. Making informed decisions is key to optimizing staffing and improving overall efficiency
Client Success Story: VMS Solution Drives Cost Savings and Transforms Staffing Operations
Seeking effective vendor-neutral strategies to modernize decision-making and compete in the talent marketplace.
How ShiftWise Flex™ is Revolutionizing Workforce Management
In today’s fast-paced healthcare environment, managing a diverse workforce can be a daunting task. Healthcare organizations face unique challenges in managing both clinical and non-clinical